The prognosis for patients diagnosed with GBM is extremely poor. Even with surgical removal of tumours followed by radiation and chemotherapy, 90 per cent of patients succumb to the disease within five years. Clearly, new therapies to tackle this deadly form of brain cancer are urgently needed.
Using mice to study Glioblastoma multiforme (GBM), the most aggressive form of brain cancer, is imperative for the discovery of new treatments. Scientists have now drastically improved this important research tool by producing an extensive catalogue of genome and transcriptome data comparing GBM tumours in humans and mice. This will help researchers to avoid biases or misleading results introduced by experimental conditions, ultimately enabling improved approaches for drug screening and the search for effective treatments for people with this devastating disease.
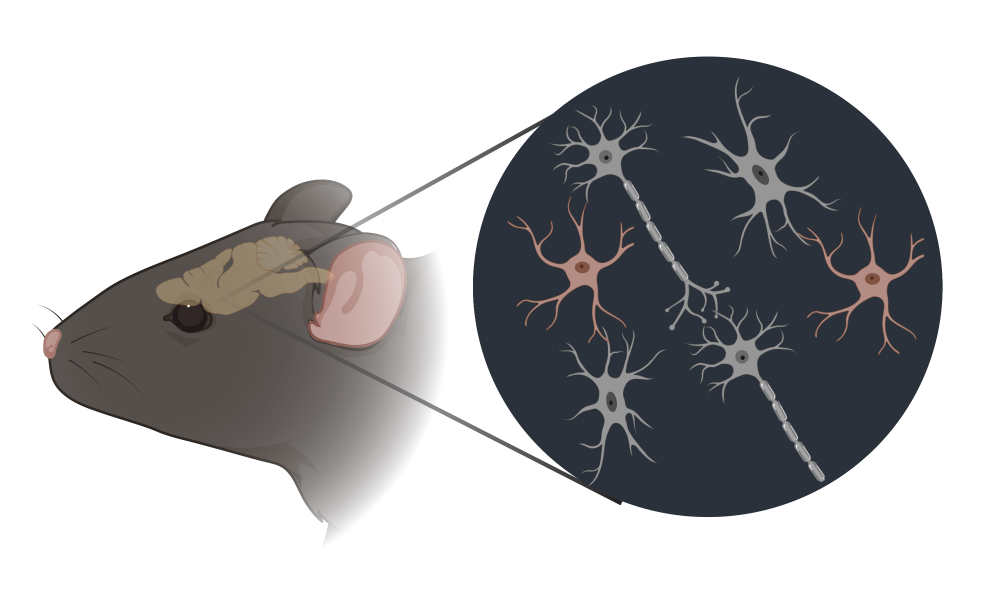
To study GBM in mice, cancer cells are taken from patients, allowed to multiply in the laboratory and are then transplanted into mice to produce what is called a xenograft. While this method is crucial for advances in GBM drug discovery, it is important to keep in mind that humans and mice differ in their biology. What cures GBM in a mouse may not work in a human.
“A significant limitation to drug discovery for GBM is that compounds that seem to work well in cell lines, don’t always work when we then try them in mouse xenograft studies,” says Dr. Steve Jones, “or worse, when compounds work in mouse studies but do not work in human patients.”
To avoid these dissappointing outcomes, scientists need a clear picture of the similarities and differences between GBM cells in patients, in a dish and in a mouse. In collaboration with scientists at the University of Calgary, the Hospital for Sick Kids, the University of British Columbia and the University of Toronto, researchers at Canada’s Michael Smith Genome Sciences Centre at BC Cancer employed their expertise in DNA sequencing and analysis to characterize the genetics of tumour cells in three differeting settings: in patients, in the laboratory and in mice. Their findings demonstrated that while the GBM mouse xenografts resembled the human disease and may provide important insights into GBM, variations in how the cancer cells behave in the different settings do exist. The wealth of information provided by this research is extremely valuable for the future study of GBM, particularly in the accurate interpretation of studies relying on this disease model.
“It will help with determining what are the druggable pathways that behave similarly between the human disease and the models, and which ones don’t,” says Dr. Jones. The findings will further enable improved approaches for drug screening, thus contributing to the search for effective treatments for this devastating disease.
“It is crucial for drugs to be tested in animal xenograft models before embarking on painstaking and time-consuming patient studies,” says Dr. Jones, “without xenograft models, drug development for cancer would likely grind to a halt.”
Background
This study was funded by the Terry Fox Research Institute and Canadian Institutes for Health Research and was published in the journal PNAS.
Learn more about brain cancer from BC Cancer.